Improve safety and precision with the right regional anesthesia needles.


Modern surgical practice has regional anesthesia as its foundation since it allows targeted pain treatment with fewer overall adverse effects. The success and safety of these approaches depend quite on one apparently tiny element: the needle. The quality, design, and exactness of the needle utilized can make a big influence from peripheral nerve blocks to spinal and epidural anesthesia.
Do you know why needles are absolutely necessary in regional anesthesia, the problems poor-quality needles can bring about, how new needle technology aids to enhance patient results, and how particular designs have special roles in various procedures. This thorough primer will assist medical device purchasers, clinicians, or original equipment manufacturer in grasping the importance of sophisticated regional anesthesia needles in hospital practice.
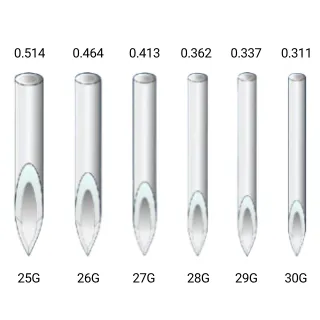
Different types of regional anesthesia—spinal, epidural, peripheral nerve block, and caudal blocks—require specific needles that suit their procedural needs. Selecting the correct type of needle is essential not only for effective anesthesia but also to minimize the risk of complications such as nerve damage or infection.
Poorly designed or low-quality needles may lead to:
Inadequate nerve localization
Tissue trauma
Post-procedural discomfort
Difficult catheter placement
Higher failure rates
For example, while the Tuohy Epidural Needle is expertly designed for precise and safe epidural anesthesia, using it incorrectly for spinal anesthesia may lead to complications such as accidental dural puncture.
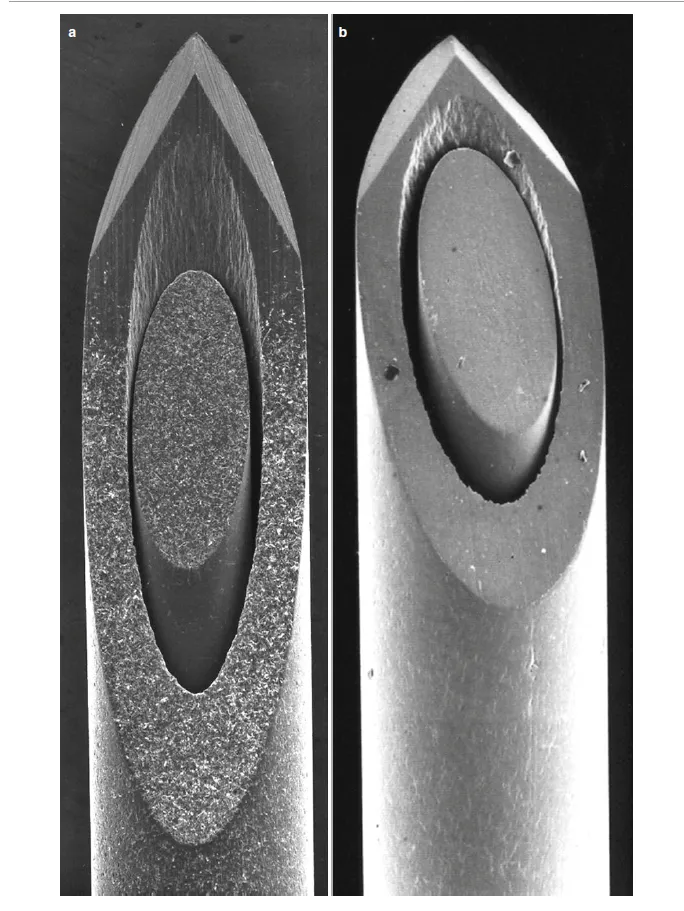
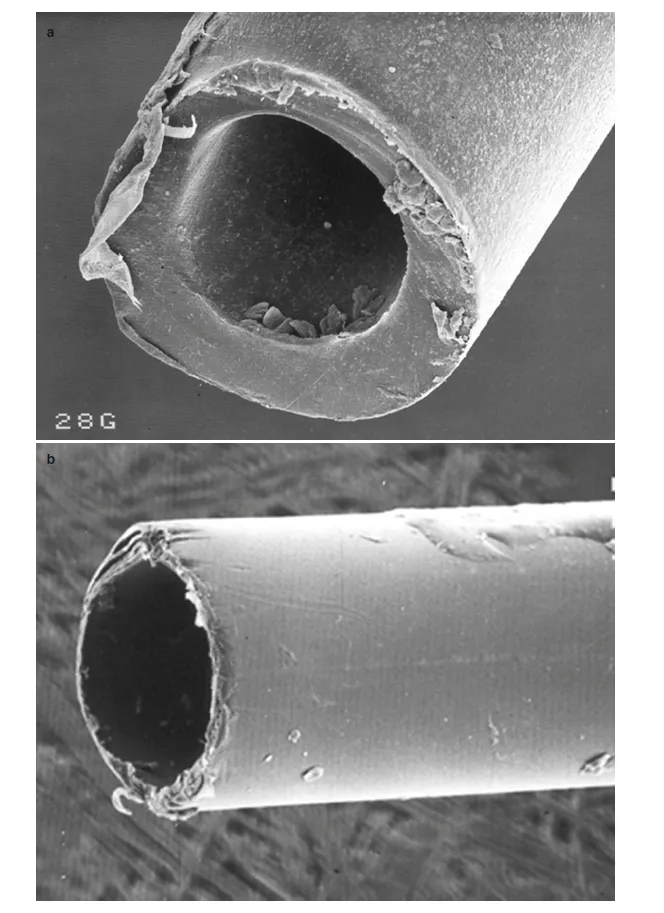
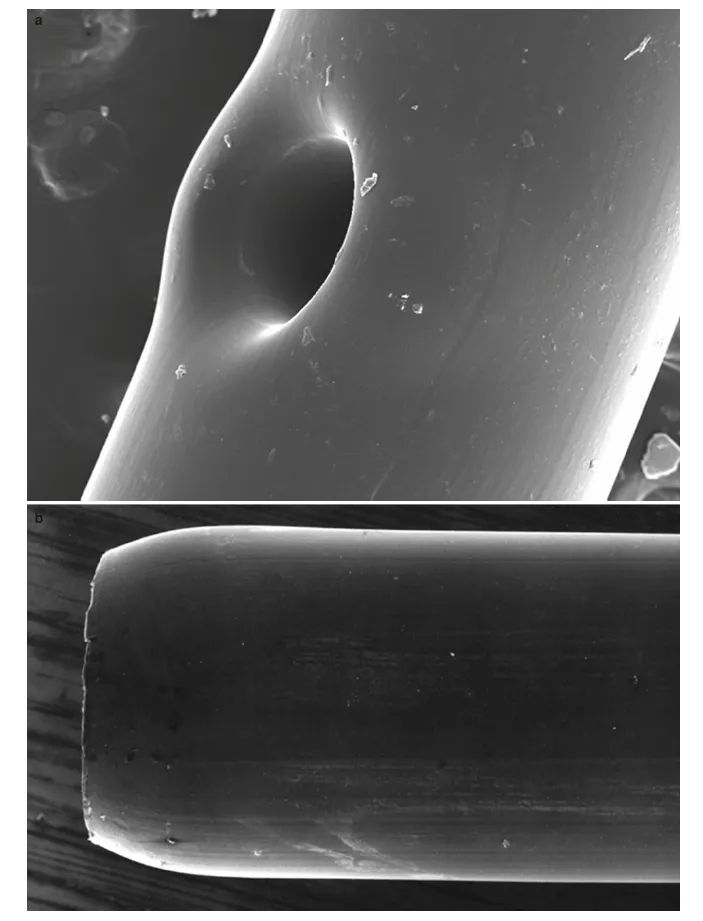
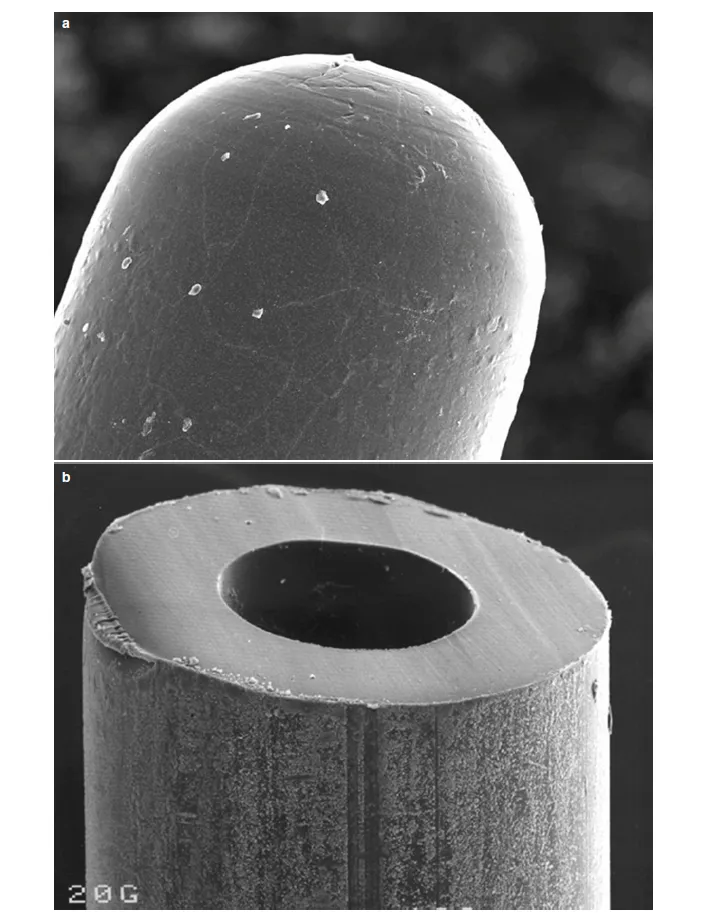
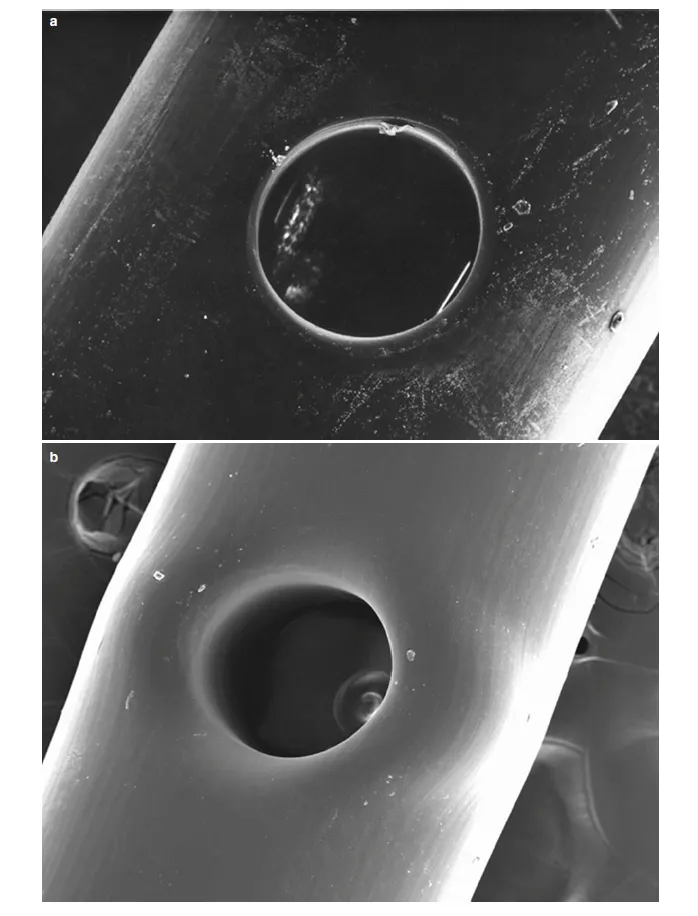
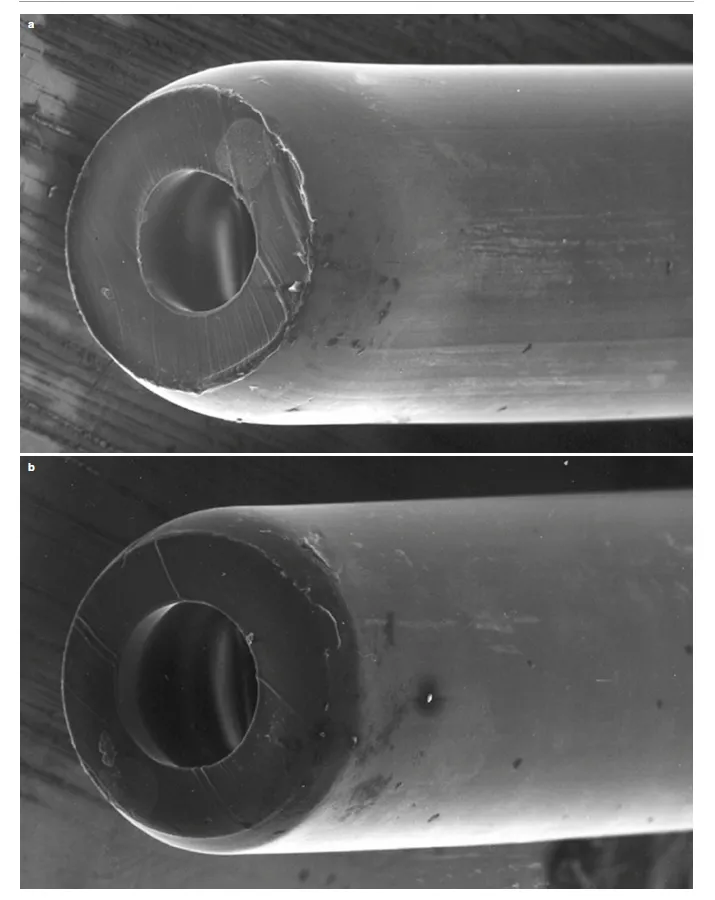
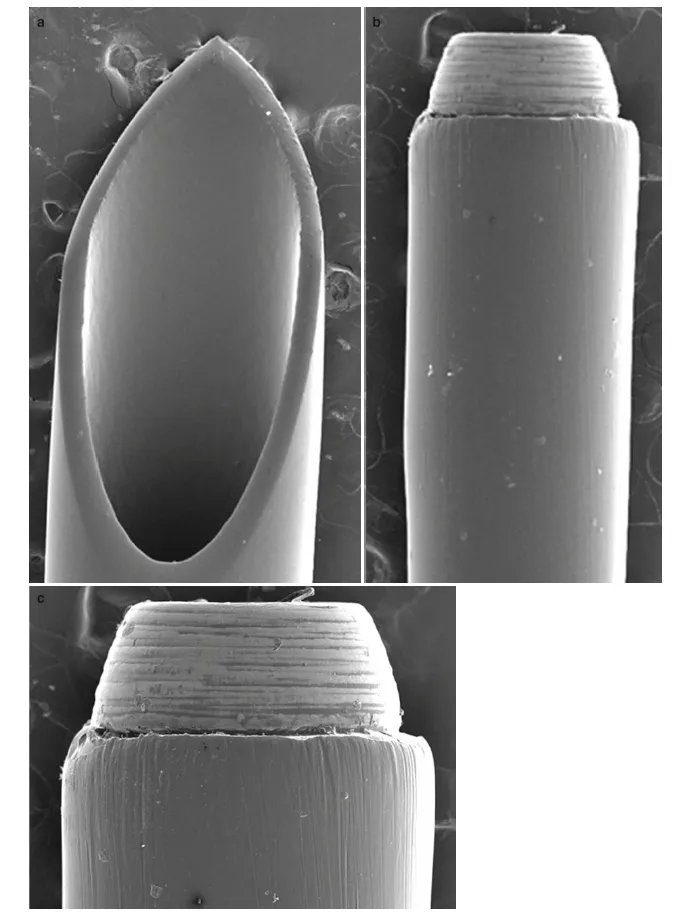
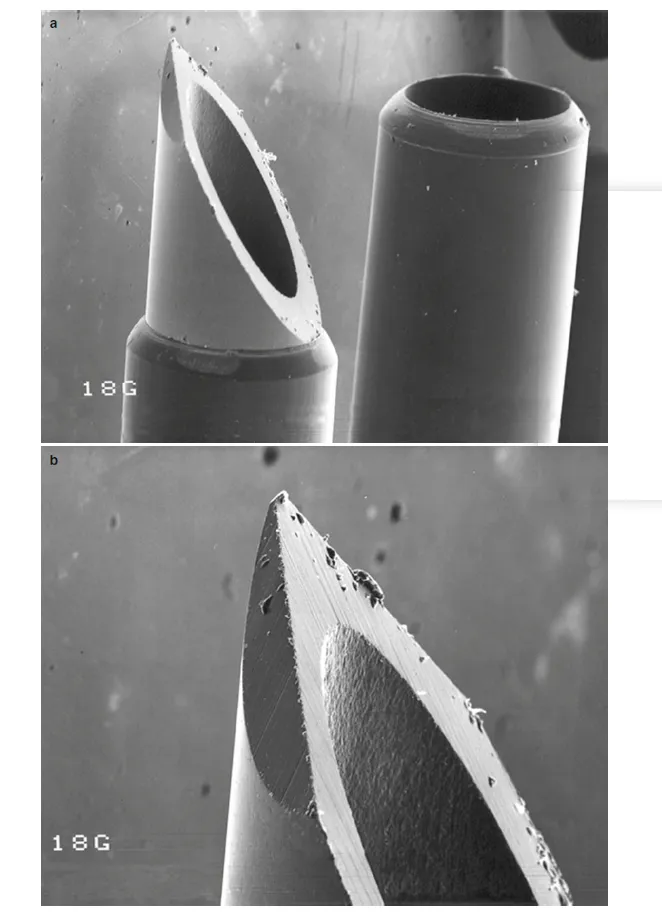
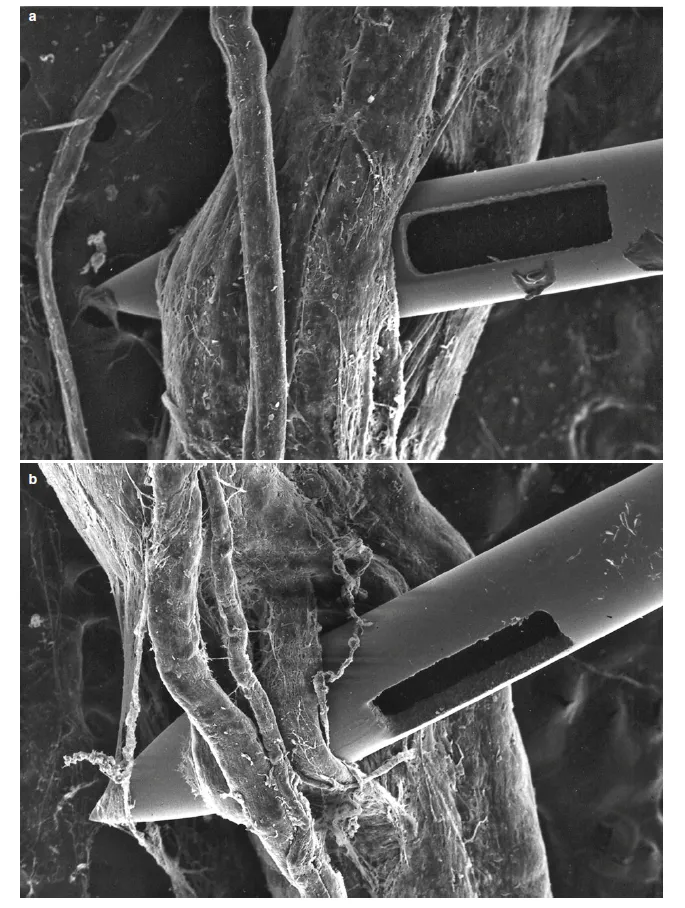
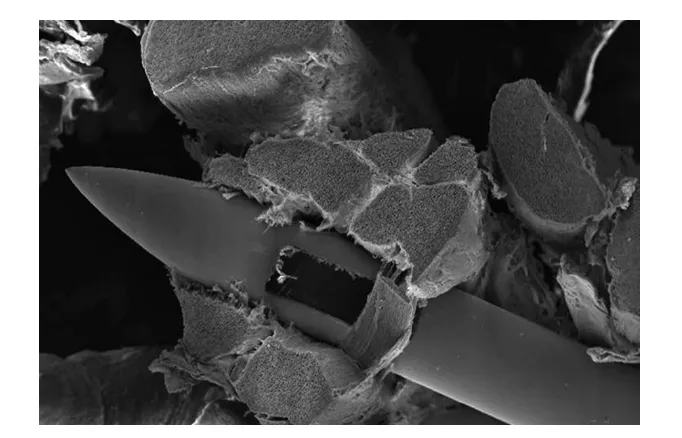
Manufacturing defects—particularly microscopic cracks or burrs at the needle tip—can cause major clinical problems. These flaws, often invisible to the naked eye, may arise during polishing or grinding stages of production. Risks include:
Fragile tips that may break during insertion
Increased trauma to tissues or nerve roots
Delayed recovery time and postoperative complications
Visual Evidence Through SEM Imaging
Using scanning electron microscopy (SEM), manufacturers and clinicians can visualize these needle tip defects, allowing:
Early identification of substandard batches
Evaluation of different suppliers
Refinement of polishing and grinding techniques
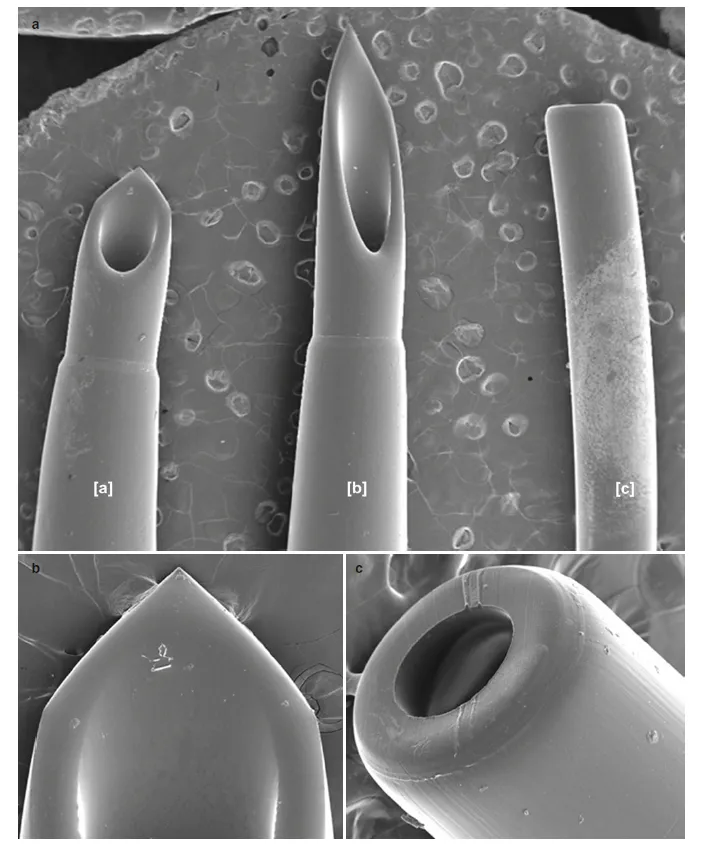
Nerve stimulation needles help anesthesiologists precisely locate nerves by emitting electrical impulses. However, not all designs are the same. Some expose too much of the needle tip, which can spread current across a larger area, making localization less accurate.
Needle design variations:
Fully exposed metal tips vs. partially insulated designs
Differences in bevel angle and length
Variability in conductivity and impedance
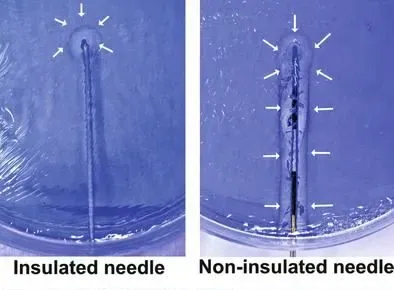
The Nerve Block Needles with optimized insulation allow accurate localization with minimal current, improving success rates and reducing patient discomfort.
Needle quality is not just a manufacturing concern—it's a patient safety issue.
Steps in Needle Quality Evaluation:
SEM analysis for micro-defects
Electrical conductivity testing
Flexibility and tensile strength analysis
Bevel angle and symmetry inspection
By integrating these quality checks, manufacturers can reduce the risk of adverse events, enhance surgical precision, and set new safety standards for the industry.
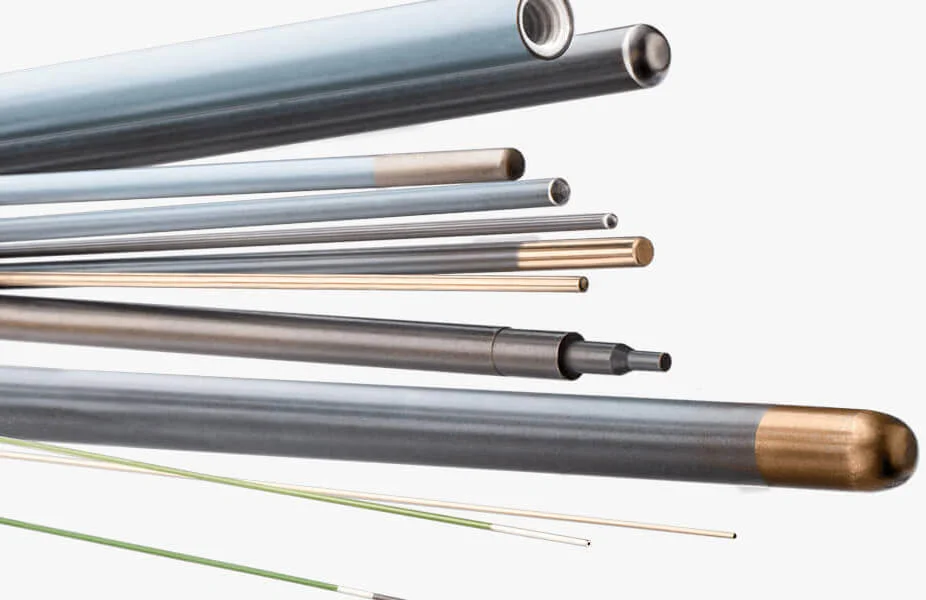
This is particularly relevant for high-precision products such as:
Echogenic Needles(ultrasound-guided needles) for ultrasound-guided blocks
Spinal Needles for intrathecal delivery
Radiofrequency Needles for pain ablation procedures



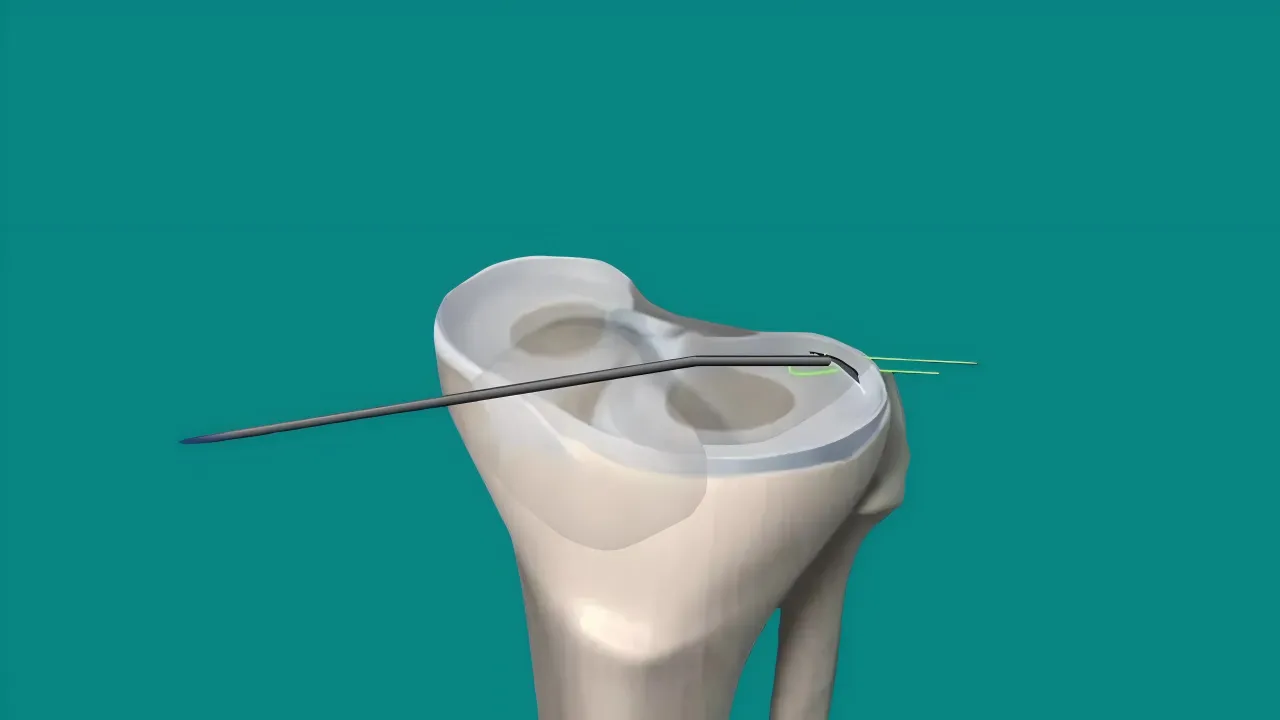
In many procedures, continuous anesthesia is required for extended pain relief. This is accomplished by inserting a catheter through the needle after localization of the nerve or epidural space.
Epidural and Subarachnoid Catheters
There are two main designs:
Open-tip catheters: A single distal opening for drug diffusion
Multi-orifice catheters: Several lateral holes and a closed tip for wider dispersion
While subarachnoid catheters are less common, they are still used in specific post-operative pain management or chronic pain scenarios. Microcatheters were once popular in the 1980s but were later discontinued due to complications such as cauda equina syndrome.
Peripheral Nerve Block Catheters
In peripheral nerve blocks, catheters are positioned adjacent to the targeted nerve to allow continuous infusion. The benefit is sustained pain control for days, allowing faster mobilization and better patient satisfaction.

During lumbar puncture or spinal anesthesia, patients may suddenly experience an “electric shock” or tingling sensation. This usually means the needle tip has contacted a spinal nerve root, triggering a depolarization reaction in the nerve axons.
This does not always indicate a misplaced needle—it often results from the needle brushing against the cauda equina rather than the conus medullaris.
Even very thin needles, such as 25G, have the potential to damage nerves. Using too much force or inappropriate needle design (e.g., overly sharp or stiff) increases the risk of:
Nerve stretch or puncture
Intraneural hematoma formation
Long-term neuropathic pain
Needles designed for atraumatic entry, such as Chiba Needles, can significantly lower the risk of tissue damage.
The anatomy of the spinal canal favors a straight sagittal approach. Deviation from this trajectory or improper patient positioning (like spine rotation) can result in off-angle insertion and inadvertent nerve contact.
Injuries can lead to:
Small vessel bleeding → hematoma formation
Inflammatory response → fibrosis
Chronic nerve conduction disorders
Therefore, needle control and careful monitoring during the procedure are essential.
If a drug is injected into the nerve sheath due to misjudged positioning, it can cause Transient Neurologic Symptoms (TNS)—including radiating leg pain or hypersensitivity.
Key prevention steps:
When electric shock is reported, withdraw needle by 2–3 mm before injecting
Use image guidance whenever possible (ultrasound or fluoroscopy)
Echogenic Needles, designed for enhanced ultrasound visibility, are critical in these cases to avoid misplacement and ensure patient safety.
Though small in size, needles are critical instruments in regional anesthesia. From engineering excellence in manufacturing to thoughtful clinical application, they influence:
Patient safety
Procedure success
Postoperative outcomes
Understanding the technical and clinical demands of anesthesia needles is vital. Investing in quality control, design innovation, and clinical collaboration will shape the next generation of safe and effective regional anesthesia tools.