CBCT-guided percutaneous lung aspiration biopsy is a highly accurate technique for the diagnosis of lung lesions, and studies have shown that its complication rate can be significantly reduced by gelatin sponge embolization.




Research on CBCT-guided percutaneous lung biopsy (PTLB/PTNB) is abundant both domestically and internationally, focusing on diagnostic accuracy, results, complication rates, and related factors. The general conclusion is that CBCT-guided PTLB is a highly accurate technique for diagnosing lung lesions.
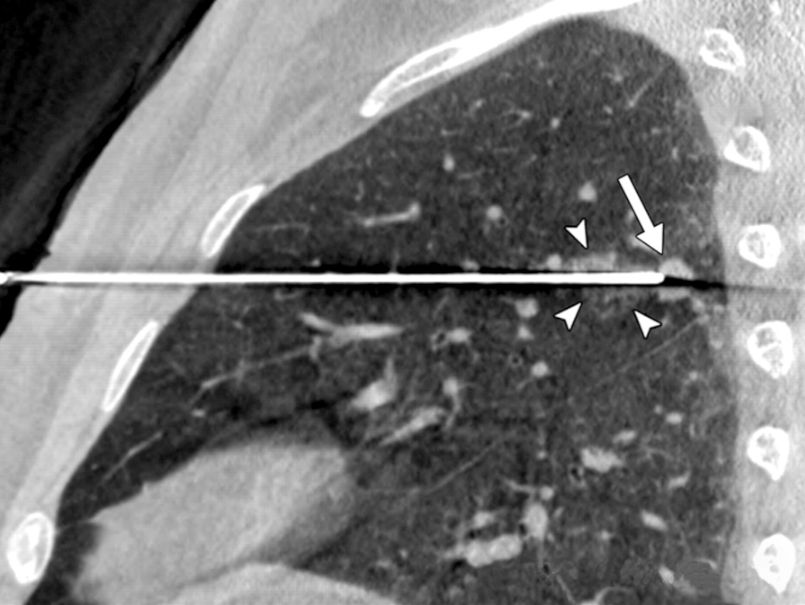
▲ Percutaneous lung aspiration biopsy
The study evaluated the incidence of pneumothorax (PTX) and pulmonary hemorrhage (PH) in PTLB and their correlation with demographic, clinical, imaging, and PTLB parameters.
Location: Department of Interventional Radiology, Zhongshan Hospital, Fudan University, Shanghai, China
Study Period: January 2019 to October 2022
Subjects: A total of 275 consecutive patients undergoing CBCT-guided PTLB were retrospectively included.
Exclusion Criteria:
1. Patients with PTX or PH found in preoperative imaging.
2. Patients with a history of PTLB.
3. Patients with target lesions located in the mediastinum, pleura, or chest wall.
4. Patients lacking postoperative CBCT images (7 patients), 24-hour post-surgery CT images (26 patients), surgical records (15 patients), pre-biopsy pulmonary thrombus (13 patients), mediastinal lesions (9 patients), iodine-125 seed implantation (3 patients), other embolic materials (8 patients), or previous punctures (2 patients). A total of 83 patients were excluded, leaving a final study population of 192 patients.
Preoperative Preparation
Patients underwent a chest plain or enhanced CT scan within a week before PTLB. Anticoagulants or platelet inhibitors were discontinued at least three days prior to surgery. Patients received breathing instructions and were advised to maintain consistent breathing during the procedure. Patients were fully informed of the necessity and potential risks of the biopsy and provided written consent.
PTLB Procedure
1. Physicians: The puncture procedures were performed by three senior interventional radiologists with over ten years of biopsy experience》
2. Method: All PTLBs were guided by a CBCT virtual navigation system under local anesthesia.
3. Instruments: A coaxial cutting needle technique was used, including an 18-gauge cutting needle and a 17-gauge biopsy coaxial cannula.
4. Positioning: Patients were placed in a supine or prone position depending on the lesion location and the presence of ribs or major blood vessels.
5. Preoperative Planning: Preoperative CBCT scans were performed to identify the safest and most accessible path to the target nodule, minimizing pleural contact and needle travel through lung parenchyma.
6. Intraoperative Operations: To reduce needle path complexity and improve accuracy, the needle angle was maintained within the rotational vertical plane during CBCT operations.
7. Sample Handling: Samples approximately 1-2 cm in diameter and 1.2 mm wide were obtained and immediately fixed in 10% formalin.
8. Treatment: For patients highly suspected of malignant lung nodules or exhibiting clinical features consistent with malignancy (e.g., combined hepatocellular carcinoma), a 17-gauge radiofrequency ablation (RFA) coaxial cannula was used instead of the biopsy cannula during PTLB. The cutting needle was removed post-biopsy, and the RFA needle was inserted through the coaxial cannula for RFA treatment.
9. Additional Procedures: Some patients received gelatin sponge slurry to embolize the needle path post-procedure. The slurry was prepared by mixing 1000-1200 μm gelatin sponge particles with 10 ml of iodinated contrast agent. After the cutting or RFA needle removal, approximately 2-3 ml of slurry was injected through the coaxial cannula under fluoroscopic guidance.
10. Postoperative Examination: Postoperative CBCT images identified any procedure-related complications. If PTX or PH was present, patients were evaluated and treated by interventional radiologists. Patients were monitored for 24 hours post-surgery, with a follow-up chest CT scan at 24 hours to detect any delayed complications.
Data Collection
Retrospective data collection included demographic, clinical, imaging, and PTLB parameters for each study participant. CT images were analyzed by two independent readers, including the PTLB operator and an attending radiologist. Nodule size was determined by measuring the maximum diameter. Nodules were classified based on characteristics, including solid, ground-glass, and cavitary.
Definitions of Several Indicators
1. Pulmonary Emphysema: Defined as any lung region (at least a trace) showing vascular and parenchymal destruction on chest CT, occupying a low attenuation space.
2. Smoking History: Classified as patients smoking at least 30 packs per year and either currently smoking or having quit within the past 15 years.
3. Pneumothorax: Based on the presence of air in the pleural cavity, classified by timing:
Immediate PTX observed on postoperative CBCT.
Delayed PTX observed on 24-hour post-PTLB CT scan.
Clinically significant PTX was defined as severe respiratory or circulatory dysfunction requiring chest tube insertion (CTI).
4. Pulmonary Hemorrhage: Defined as ground-glass opacity in the lung parenchyma due to alveolar filling with blood. PH was categorized into four groups:
Asymptomatic
Mild hemoptysis (less than 100 ml within 24 hours)
Moderate hemoptysis (100-500 ml within 24 hours)
Severe hemoptysis (more than 500 ml within 24 hours)
Clinically significant PH required invasive medical interventions such as bronchoscopy or endovascular treatment to achieve hemostasis.
Statistical Methods
Statistical analysis was performed using SPSS software (version 27.0; SPSS Inc., Chicago, IL). Subgroup analyses identified significant factors using Student's t-test for continuous variables and Pearson's chi-square test for categorical data. Due to the limited sample size, Fisher's exact test was used. Logistic regression analysis was then employed to further determine the impact of evaluated parameters on the likelihood of developing PTX and PH. Results were reported as odds ratios (ORs) with 95% confidence intervals. A p-value of less than 5% (p < 0.05) was considered statistically significant.
Baseline Clinical Characteristics and PTLB Parameters
The demographic, clinical, imaging, and procedural parameters of patients are summarized in Table 1. A total of 192 patients underwent PTLB (129 males, 67.2%), with an average age of 62.1 ± 13.4 years.
Among all patients, 29 (15.1%) had a smoking history, and 47 (24.5%) were diagnosed with pulmonary emphysema. Among patients with emphysema, 16 (34.0%) later experienced postoperative PTX. The mean diameter of lung lesions was 3.40 ± 2.20 cm, with 51 patients (26.6%) having lesions in the left upper lobe.
Nodule detection is shown in the figure, with solid nodules being the most common (85.4%).
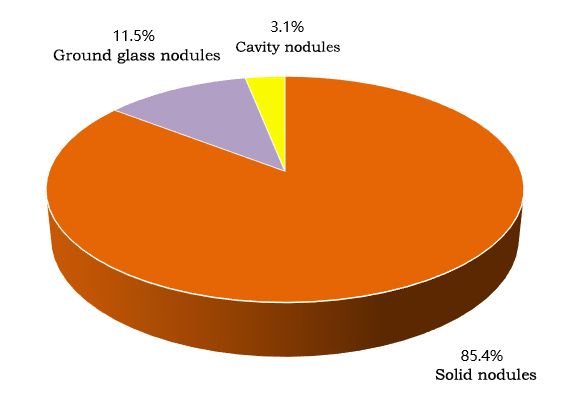
▲ Nodule detection
During PTLB, 43 patients (22.4%) underwent RFA post-PTLB. Gelatin sponge was used to seal the puncture path in 77 patients (40.1%).
In the pathological biopsy performed post-PTLB, 3 patients (1.6%) were undiagnosed due to insufficient material.
Among the 192 patients, the final diagnosis is shown in the figure, with 141 diagnosed as malignant tumors (73.4%), including 113 primary lung cancers and 28 metastatic lesions.
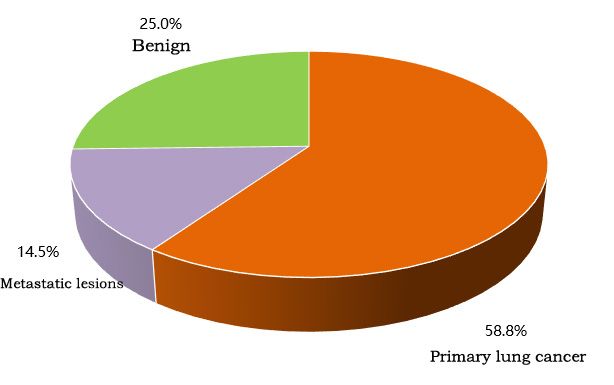
▲ Final diagnosis
Complications
Pneumothorax: Observed in 67 patients (34.9%).
Immediate CBCT scan: 42/67 (62.7%)
24-hour CT scan: 25/67 (37.3%)
Most PTX cases resolved spontaneously, but 5 patients required CTI (7.5%), with an average catheter placement duration of 2.6 ± 0.9 days. Due to the limited number of patients requiring CTI, no regression analysis was performed to examine influencing factors for CTI.
Pulmonary Hemorrhage: Occurred in 63 patients (32.8%).
Asymptomatic: 39/63 (61.9%)
Mild hemoptysis: 15/63 (23.8%)
Moderate hemoptysis: 9/63 (14.3%)
Severe hemoptysis: 0/63 (0%)
Moderate hemoptysis patients improved with appropriate hemostatic treatment. No patient experienced severe hemoptysis requiring invasive medical intervention.
Subgroup Analysis
Subgroup analysis results for PTX and PH are shown in the figure. The analysis indicated that the incidence of PTX was associated with lesion diameter, use of gelatin sponge, and RFA (p < 0.05). PH was associated with the presence of pulmonary emphysema, lesion diameter, use of gelatin sponge, RFA, and the number of samples extracted (p < 0.05).
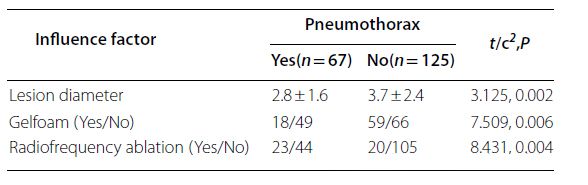
▲ Subgroup analysis results of PTX
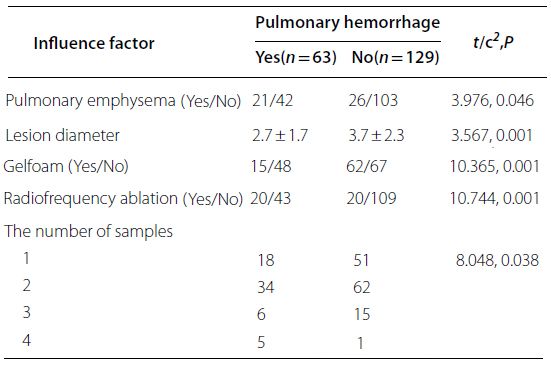
▲ Subgroup analysis results of PH
Logistic Regression Analysis
Include significant factors from subgroup analysis in logistic regression analysis. The results of logistic regression analysis, shown in the figure, assess the impact of parameters on PTX and PH.
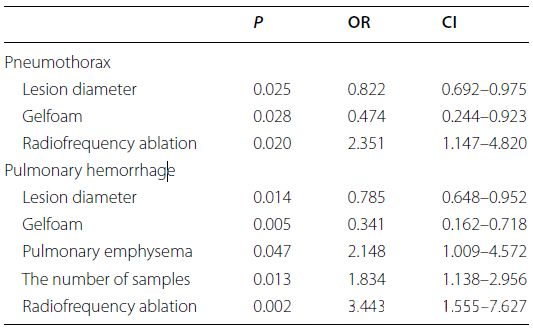
▲ Logistic regression analysis of significant factors in subgroup analysis
Logistic regression analysis identified lesion diameter (OR per cm = 0.822), use of gelatin sponge (OR = 0.474), and radiofrequency ablation (RFA) treatment (OR = 2.351) as potential influencing factors for PTX. For PH, lesion diameter (OR per cm = 0.785), use of gelatin sponge (OR = 0.341), presence of emphysema (OR = 2.148), sample number (OR per additional sample = 1.834), and RFA treatment (OR = 3.443) were considered potential influencing factors. The odds ratio (OR) indicates the odds of the dependent variable occurring with each unit change in the independent variable.
Advantages of percutaneous needle biopsy (PTNB) assisted by CBCT: Real-time imaging during needle insertion simplifies trajectory planning, enhances accuracy in reaching target lesions, and potentially reduces operation time and patient radiation dose.
Impact of PTX and PH: PTX and PH significantly affect patient management and discomfort levels. Mild cases may prolong hospital stay, while severe cases pose substantial risks to respiratory and circulatory systems.
Incidence of PTX and PH: In this study, PTX and PH incidences were 34.9% and 32.8%, respectively, consistent with previous literature on CT-guided procedures. Conservative treatments were effective in most cases of PTX and PH. Only 7.5% of cases required chest tube insertion, aligning with reported rates ranging from 2.4% to 15%. No PH patients required bronchoscopy or intravascular treatment. Furthermore, no significant complications such as liver or spleen injury, air embolism, or death were observed in the study, indicating that CBCT-guided PTNB is relatively safe, with low incidence of clinically significant complications and minimal need for prolonged hospital stay for most patients.
Factors associated with PTX and PH occurrence: While many factors including demographics, clinical characteristics, imaging findings, and PTNB parameters were considered, only a few (lesion diameter, use of gelatin sponge, RFA, and number of samples extracted) showed statistically significant results.
Factors reducing PTX and PH occurrence: A key finding was the significant reduction in PTX and PH incidences with the use of gelatin sponge (OR reducing by 56.8% and 69%, respectively). This finding is clinically significant due to the accessibility and simplicity of gelatin sponge use in medical practice. Interventional radiologists have explored various techniques to mitigate complication risks since the inception of PTNB. Injection of gelatin sponge causes it to expand within the needle track, forming a dense plug conforming to the track shape, effectively preventing bleeding, pulmonary air entry through the puncture track, and pleural rupture. Renier et al. successfully reduced PTX and CTI rates by closing puncture tracks with a mixture of 15 pieces of absorbable gelatin sponge (2×6 cm) and 2 ml saline. Unlike previous studies, our study used smaller gelatin sponge particles ranging from 1000 to 1200 micrometers. This method not only reduced preparation time but also allowed denser closure of puncture tracks. Larger diameters showed protection against PTX and PH, with ORs per cm of 0.822 and 0.785, respectively.
An increased number of samples extracted during PTNB was associated with a higher likelihood of PH occurrence, corresponding OR increasing by 83.4% per additional sample.
Biopsy of large lesions is easier, with shorter needle placement time in substance, and lower likelihood of complications. Conversely, obtaining samples from repeated punctures may be challenging, requiring longer operation time and higher risk of complications. The study indicates that performing RFA treatment after PTNB is associated with increased risks of PTX and PH (ORPTX = 2.351; ORPH = 3.443). Previous studies suggest that performing PTNB and RFA treatment in the same surgery can avoid multiple punctures. Therefore, highly suspicious patients with malignant lung nodules underwent RFA after PTNB in the study.
Schneider et al. noted in their study report that immediate biopsy before RFA may lead to PH or PTX because biopsy can blur or displace tumors, affecting the accuracy of subsequent RFA needle placement. This is due to the lack of appropriate guidance sheaths during biopsy, requiring additional punctures. However, in our study, due to the use of multi-functional coaxial sheaths, punctures were required during establishment of puncture channels, after PTNB, only the cutting needle was removed, and the coaxial sheath remained in place. This approach ensures the accuracy of pathological results and reduces the number of punctures required.
Izaaryene et al. conducted a pathological study of pig lungs after radiofrequency ablation (RFA), observing distinct needle tracts compared to simple biopsy. They found unique histological changes in the ablation tract, which may be attributed to thermal effects. This study suggests that needle tracts formed after RFA may remain open longer, potentially leading to PTX and PH compared to biopsy alone.
Furthermore, the study revealed that biopsy after radiofrequency ablation (RFA) treatment may increase the risk of PTX and PH, consistent with previous research findings. Heat generated by RFA treatment may affect closure of the needle tract, increasing complication risks. The study also found that the presence of emphysema increases the risk of PH, possibly due to pulmonary hypertension or structural damage to lung tissue, providing more space for PH extension.
Limitations: Firstly, this was a retrospective study, limited by available surgical records, preventing further exploration of multiple influencing factors such as distance between puncture points and lesions. Secondly, being a single-center study may limit the generalizability of results. Thirdly, the number of patients requiring chest drainage tubes, bronchoscopy, or intravascular treatment was limited, restricting comprehensive analysis of factors influencing these interventions.
Conclusion: CBCT-guided PTNB is a reliable technique widely used for diagnosing pulmonary lesions. However, like CT-guided PTNB, PTX and PH remain prominent complications. To reduce these complications, this study introduces an innovative and feasible method—using gelatin sponge to seal puncture paths. This method has shown significant reduction in complication rates.