Learn about the types, implantation procedures, and benefits of cardiac pacemakers for treating various heart conditions in this comprehensive guide.




A cardiac pacemaker is an electronic therapeutic device implanted within the body. It uses a pulse generator powered by a battery to send electrical impulses through lead electrodes to stimulate the heart muscle. This stimulation causes the heart to contract, thereby addressing heart function disorders caused by certain arrhythmias.

Since the first pacemaker implantation in 1958, the technology and manufacturing processes have rapidly evolved, with pacemakers becoming increasingly sophisticated. While pacemakers have successfully treated thousands of patients with bradyarrhythmias, their application has expanded to treat tachyarrhythmias and non-electrical cardiac diseases. These include preventing paroxysmal atrial tachyarrhythmias, carotid sinus syncope, and biventricular synchronized therapy for drug-resistant congestive heart failure. This article provides a comprehensive overview of cardiac pacemakers.
Cardiac pacemakers are typically implanted in patients with bradycardia, tachycardia, arrhythmia, cardiac arrest, heart failure, and atrial fibrillation.
Bradycardia: A condition characterized by abnormally slow heartbeats. Pacemakers are implanted to address this issue. In healthy adults, the heart beats 50 to 80 times per minute. In patients with bradycardia, the heart beats less than 50 times per minute, failing to pump sufficient oxygen-rich blood to the body.
Tachycardia: A condition associated with an abnormally high heart rate (over 100 beats per minute at rest). The heart cannot effectively pump blood to other organs. In this case, an Implantable Cardioverter Defibrillator (ICD) is used.
Arrhythmia: Refers to irregular heartbeats that impair effective pumping. Cardiac Resynchronization Therapy (CRT) devices are preferred in these situations.
Atrial Fibrillation: The most common type of arrhythmia, where the atria contract too quickly and asynchronously. A CRT device combined with a pacemaker (CRT-P) can be used.
Cardiac Arrest: In such cases, an ICD is recommended.
Heart Failure: Often due to damaged heart muscle failing to pump effectively. A CRT device combined with a defibrillator (CRT-D) is used.
There are three main types of implantable cardiac pacemakers: Cardiac Resynchronization Therapy devices (CRT), pacemakers, and Implantable Cardioverter Defibrillators (ICD).
3.1 Cardiac Resynchronization Therapy Devices (CRT)
CRT devices send small electrical impulses to both lower chambers of the heart to help them beat more synchronously, allowing the heart to pump oxygenated blood more efficiently. Depending on the patient’s heart failure condition, two types of devices are used:
CRT-P (Cardiac Resynchronization Therapy Pacemaker)
CRT-D (Cardiac Resynchronization Therapy Defibrillator)

3.2 Pacemakers
Pacemakers send electrical signals to the heart to increase its rate, alleviating bradycardia symptoms.

3.3 Implantable Cardioverter Defibrillators (ICD)
ICDs monitor the heart rhythm continuously. If the heart beats too fast or irregularly, the device sends small electrical signals to correct it. If the rapid heart rate persists, the ICD delivers a shock to restore a normal rhythm.

Implanting a cardiac pacemaker does not require open-heart surgery. The device is placed under the skin in the area below the collarbone. Most patients can go home within 48 hours after the procedure, which takes about an hour. The steps are as follows:
Administering local or general anesthesia if necessary.
Making a 5-10 cm incision in the upper chest below the collarbone.
Inserting one or more leads through a vein (femoral or subclavian) into the heart and connecting them to the pacemaker.
Programming and testing the medical device, inserting the pacemaker in the chest, and suturing the incision.
The lithium-iodine battery in a cardiac pacemaker typically lasts 6 to 8 years and weighs less than 30 grams. Replacing the battery involves making a new incision at the site of the old one and swapping out the battery pack. The leads are generally left in place indefinitely unless complications, such as infection, occur.
Risks can occur during the surgery or after the pacemaker is implanted.
Surgical Risks:
Anesthesia-related risks
Bleeding
Damage to nearby structures (tendons, muscles, nerves)
Puncture of the lung or vein
Heart damage (perforation or tissue damage)
Severe arrhythmias
Heart attack
Blood clot formation
Death
Post-implantation Risks:
Infection
Skin erosion near the device
Device migration from its initial position
Lead dislodgement
Stimulation of surrounding tissues (including heart tissue and nerves) by the lead electrodes or pulses
Device malfunction due to mechanical impact or electromagnetic interference
7.1 Medtronic
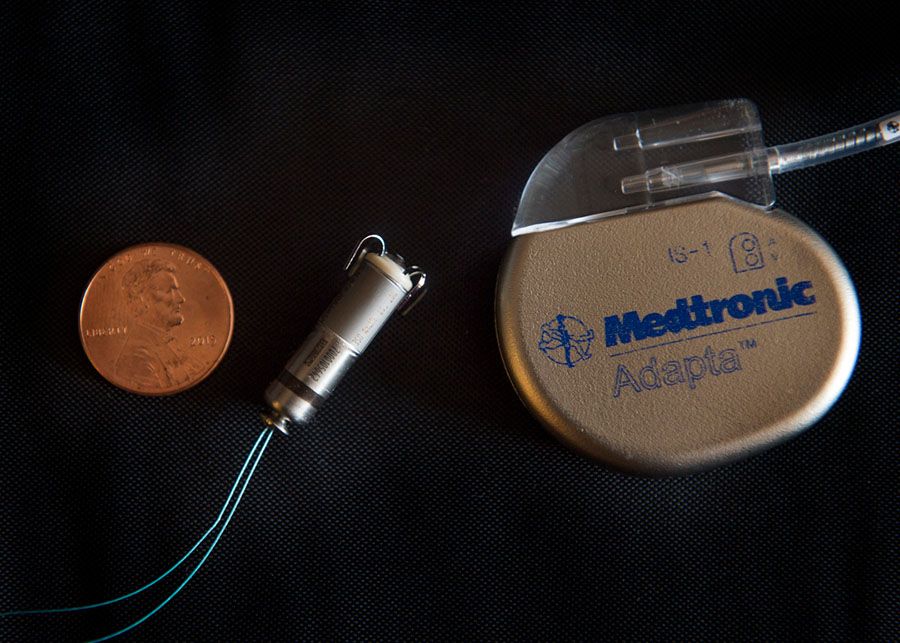
A leader in cardiac care, Medtronic offers seven series of cardiac pacemakers, including permanent implantable pacemakers, temporary external pacemakers, and the world's smallest leadless pacemaker, Micra.
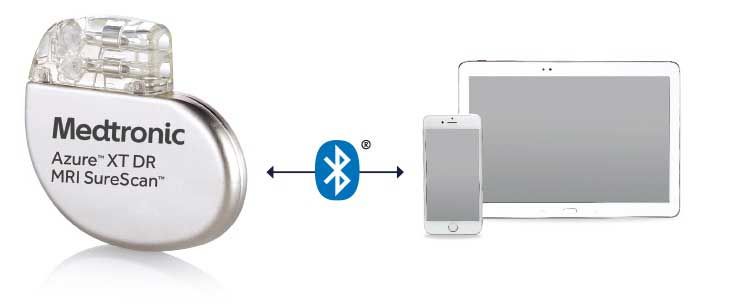
Azure: Uses Bluetooth technology for remote monitoring via a smartphone app, enhancing patient engagement with their health and reducing clinic visits. It also features a highly accurate atrial fibrillation management algorithm (96% accuracy).
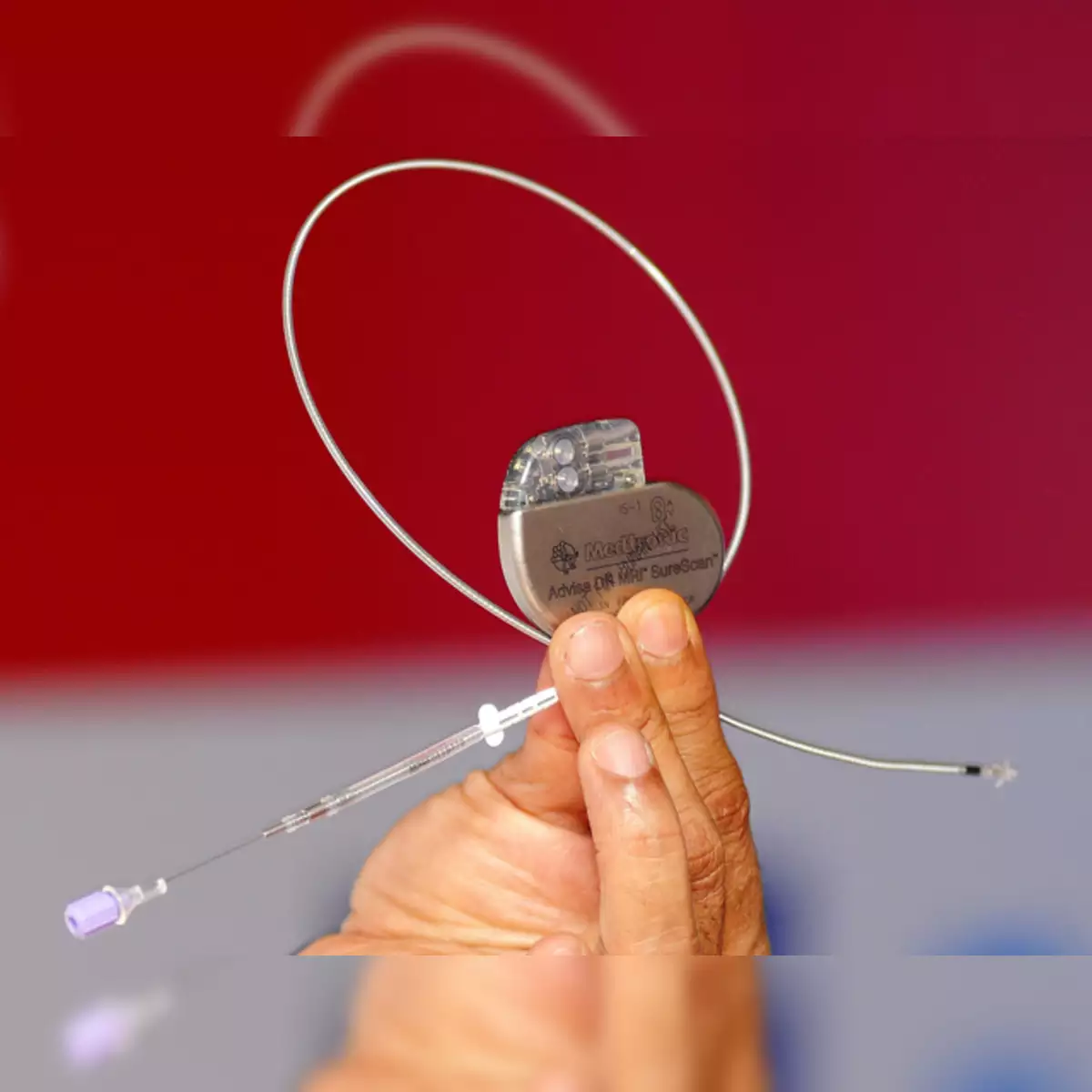
Advisa: MRI-compatible pacemakers, resolving MRI interference issues, suitable for 1.5T and 3T full-body MR scans. Available in single-chamber (SR) and dual-chamber (DR) models.
Adapta: Combines physiological and automatic pacing to reduce unnecessary right ventricular pacing by 99%. The DR model is the first pacemaker with Managed Ventricular Pacing (MVP) technology.
7.2 Abbott
After acquiring St. Jude Medical, Abbott has become a significant player in cardiac rhythm management, known for its compact pacemakers, all around 10 cm³ in volume.
Assurity: The world's smallest MRI-compatible pacemaker with a lifespan of up to 10 years, minimizing the risk of infection and complications from device replacement. It's one of the thinnest devices on the market, designed for smaller surgical incisions.

7.3 Boston Scientific
A leader in the interventional field, Boston Scientific's ACCOLADE series pacemakers offer the most MRI programmable options with no scanning time limitations and no patient restrictions. These devices also have a lifespan of up to 13 years, and the post-operative monitoring system facilitates patient follow-up.

By understanding the different types and applications of cardiac pacemakers, healthcare providers and patients can make informed decisions about the most suitable treatment options for various heart conditions.