Discover the crucial implant design factors for zero bone loss, including the importance of smooth necks and micro-gaps, and how platform switching can prevent bone resorption.




Zero Bone Loss and Alveolar Crest Bone Stability
Zero bone loss, or alveolar crest bone stability, refers to the condition where the crest bone does not experience any recession or loss for any reason. To achieve this goal, there are two critical implant design factors: whether the implant neck is smooth and whether there is a micro-gap at the implant-abutment connection.
1.1 History of Smooth Necks
In the past, implant necks were designed with mechanically polished smooth surfaces to reduce plaque accumulation if the implant was exposed to the oral environment due to bone loss. However, clinical studies have shown that bone tissue in contact with smooth surfaces tends to absorb.
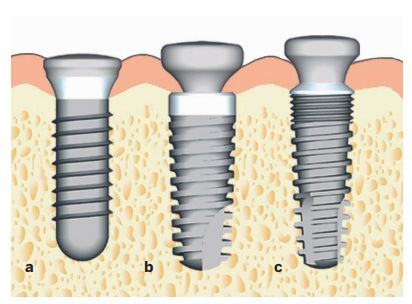
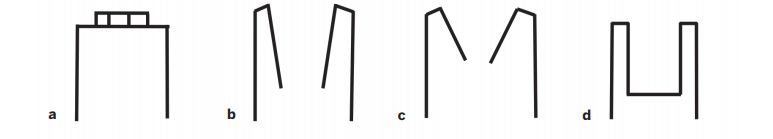
Different implant neck types
a-rough surface, b-smooth surface, c-micro-threaded. Studies have shown that smooth surface necks experience the most bone loss, while micro-threaded necks experience the least.
1.2 Mechanism of Bone Resorption with Smooth Necks
Mechanically polished implants cannot effectively distribute occlusal stress, leading to stress shielding and subsequent bone loss. During the second-stage surgery, bone growth can be observed on the implant, but after functional loading, the bone will resorb to the first thread of the implant. Thus, bone loss associated with smooth necks can be described as non-functional bone resorption. Although smooth necks may lead to bone resorption, this does not mean the implant will fall out. However, it is still advisable to minimize such resorption by placing the smooth neck at the bone level since the bone will eventually resorb to the junction of the smooth and rough surfaces.
Question: Some might wonder how stress is distributed on early fully machined Branemark implants. Although these implants are polished (or mechanically machined), the threads embedded in the bone can still distribute stress to the bone.
All two-piece implants have a micro-gap at the implant-abutment connection. The micro-gap presents two main issues: bacterial contamination and micro-movement.
2.1 Bacterial Contamination
Two-piece implants inevitably have internal contamination since small amounts of saliva or blood can enter the implant and cannot be removed by conventional methods.
2.1.1 Size of the Micro-Gap
In tapered connection implant systems, the micro-gap is only 0.5 microns, smaller than the diameter of microorganisms, making it a sterile connection. However, if micro-leakage occurs at the implant-abutment interface, the entire implant system can become contaminated with microorganisms.
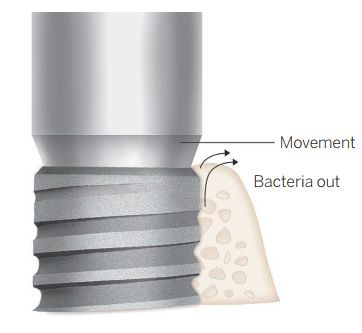
Micro-leakage at the implant-abutment interface
If the implant-abutment connection is at the bone level and becomes contaminated, the bone will be infected by bacteria leaking from the implant, leading to bone loss. The size of the micro-gap and the stability of the connection are crucial factors in bone loss.
2.1.2 Stability
Implant-abutment connections come in different types, including external connections, platform matching, and internal connections. Tapered connections seem to provide the best stability, especially when the implant is placed below the alveolar crest.
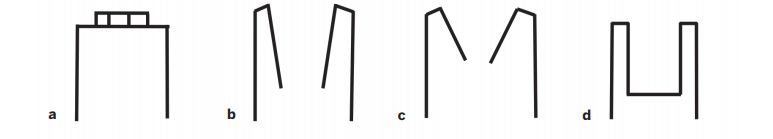
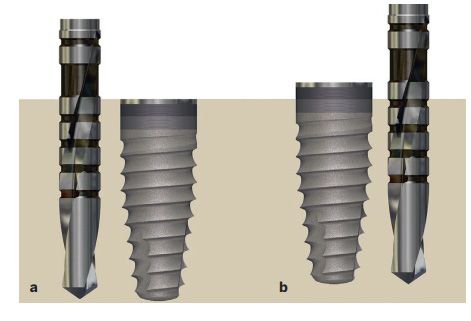
Different types of implant-abutment connections
a-external connection, b-5-6 degree tapered connection, c-8-20 degree tapered connection, d-internal connection.
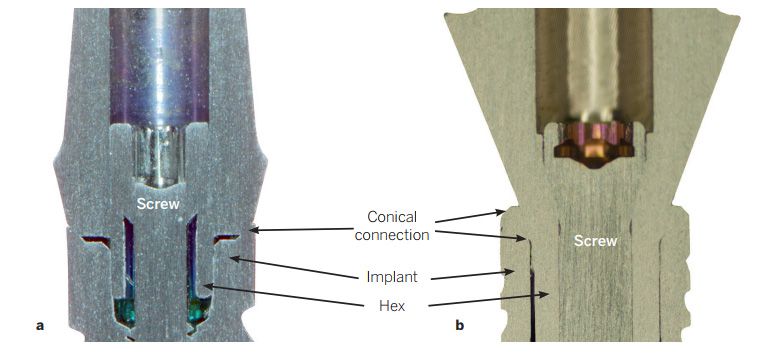
Different types of implant-abutment connections
a-45-degree short internal taper connection, b-15-degree tapered connection. The tapered connection is the only point of contact and stress distribution between the abutment and the implant.
Bacteria and micro-movement within the implant cause microbial leakage at the implant-abutment interface, leading to inflammatory cell infiltration in the soft tissue around the micro-gap. This infiltration, known as the abutment-related connective tissue infiltration zone, might be a host defense mechanism around the bone.
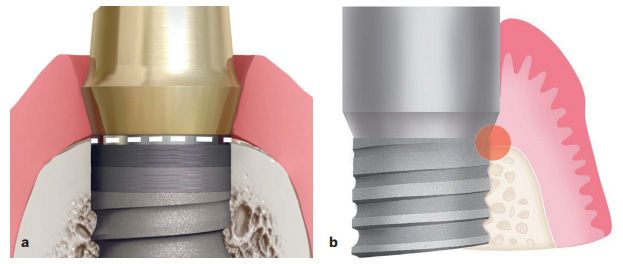
Implant-abutment interface placed at or near the bone level
The image above shows improperly placed non-platform-switched implants. a-The micro-gap is almost at the bone level, b-Micro-movement and bacterial contamination cause an inflammatory reaction.
2.2 Position of the Micro-Gap
2.2.1 Bone-level Placement of Platform Matching Implants
Platform matching implants placed above the bone level move the micro-gap away from the bone to reduce alveolar and crest bone resorption.
Research shows that in thick gingival biotypes, bone loss around implants placed above the bone level is 0.68 mm, less than that of implants placed at bone level. However, this still represents significant bone resorption, likely due to the exposure of the rough surface above the bone level, leading to plaque accumulation. Therefore, platform matching implants placed at the alveolar crest bone level should have a 0.5-1mm smooth neck.
Implants placed below and above the alveolar crest
a-When non-platform-switched implants are placed at or below the alveolar crest, micro-gap micro-movement and bacterial contamination occur within the bone, b-Placing implants above the alveolar crest can reduce the impact of these factors on bone.
2.2.2 Placement of Platform-Switched Implants
Platform switching allows bacteria to migrate horizontally inward and away from the bone tissue. Platform switching refers to the concept where the diameter of the abutment or superstructure is smaller than that of the implant platform.
Special note: The difference between the abutment and implant platform should be at least 0.4mm. If the difference is less than 0.4mm, the bacterial infiltration range will not be far enough from the bone, making the platform switching ineffective, similar to standard implants.
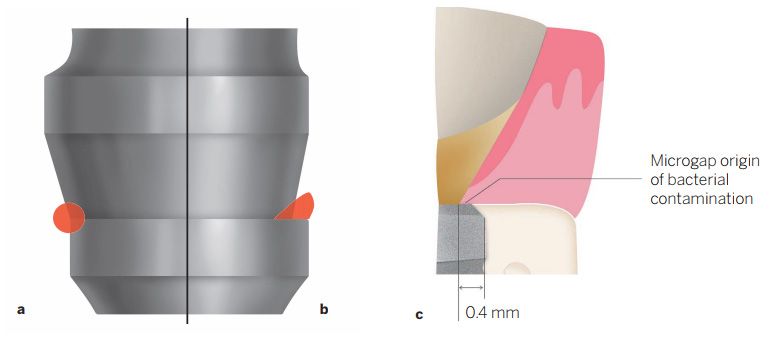
Non-platform-switched and platform-switched implants
a-In non-platform-switched implants, bacteria leak directly into the bone from the micro-gap, b-The advantage of platform switching is that bacteria migrate inward and away from the alveolar bone, c-The difference in platform switching is crucial, with at least a 0.4mm differential for effectiveness.
2.3 Micro-Movement
Preventing bacterial contamination is one factor in maintaining alveolar crest bone stability, and reducing micro-movement is another. Generally, the smaller the taper, the more stable the connection, with better resistance to lateral movement. However, overly small taper connections can hinder the placement of fixed bridge restorations, which is a drawback.
Different types of implant-abutment connections
The first type, with a Morse taper angle of 2-4 degrees, is used by well-known implant brands like Ankylos and Bicon. The second type is a broad taper connection with an angle of 5-20 degrees, commonly used by Straumann, Nobel Biocare, MIS, and other brands. The third type has a taper angle exceeding 20 degrees, which is actually referred to as an internal or flat connection rather than a taper connection.
Smooth necks do not promote bone integration and placing them below the bone level will inevitably lead to bone loss.
Micro-gaps lead to bacterial leakage and micro-movement at the implant-abutment connection, causing bone damage.
Platform switching moves the micro-gap inward horizontally, keeping bacterial leakage away from the bone.
Tapered connections ensure the stability of the implant-abutment connection, but this stability alone cannot prevent bone loss.